Coronary and valvular heart disease
Liberal or restrictive oxygenation, GLP-1 agonist therapy, edoxaban and spironolactone.
Research from four abstracts highlight oxygenation strategies, DOACs and novel agents to optimize cardiac surgery and outcomes post-myocardial infarction. They found that:
- Liberal or restrictive oxygenation may be safe for patients undergoing cardiopulmonary bypass-assisted coronary artery bypass grafting or aortic valve replacement.
- Perioperative novel exenatide, a GLP-1 agonist therapy, did not benefit cardiac surgery patients.
- Edoxaban shows clinical benefit in patients after bioprosthetic valve replacement.
- Spironolactone may reduce heart failure but did not reduce primary outcomes in patients after acute myocardial infarction.
Liberal or conservative oxygenation strategy during cardiac surgery may be considered
Adequate oxygenation is essential for preserving organ function during coronary artery bypass grafting or aortic valve replacement surgery. Traditionally, high levels of oxygenation have been applied during extracorporeal circulation. Still, a conservative or liberal oxygenation strategy could be considered for patients undergoing these surgical interventions, according to the Efficacy of Restrictive versus Liberal Oxygenation in Patients undergoing Coronary Artery Bypass Grafting or Aortic Valve Replacement, results of one of two co-primary interventions independently investigated in the GLORIOUS trial.
The 2-by-2, single-center clinical trial randomized 1,400 patients undergoing elective or subacute coronary artery bypass grafting and/or surgical aortic valve replacement from 2016 to 2021 to a conservative oxygenation strategy of 50% fraction of inspired oxygen (FiO2) versus a liberal oxygenation strategy of 100% FiO2 during cardiopulmonary bypass surgery and for the first hour after weaning.
The primary outcome was time to the first occurring composite endpoint during follow-up, including death, renal failure requiring renal replacement therapy, stroke, new onset heart failure or any readmission for heart failure. The trial was designed as event driven, and accordingly, the follow-up period was a priori defined to continue until a total of 323 events had occurred. Secondary endpoints included predefined safety endpoints during the index admission, such as surgical site infection, acute kidney injury, hypoglycemia, pancreatitis, a relative reduction of ejection fraction of 50% compared to baseline, reoperation for bleeding and any cause and post-surgical myocardial infarction. Additionally, re-admission for cardiovascular causes within 12 months was monitored. Sebastian Wiberg, MD, PhD
Sebastian Wiberg, MD, PhD
Overall, oxygenation at 50% versus 100% did not affect the composite endpoint of organ injury in adults undergoing cardiopulmonary bypass-assisted cardiac surgery after a median follow-up of 5.9 years.
“The neutral results of our trial suggest that it’s safe to only administer 50% oxygen during cardiopulmonary bypass and that if you are worried about end-organ perfusion, it’s also safe to administer 100% oxygen,” said Sebastian Wiberg, MD, PhD, clinical associate professor at Copenhagen University Hospital Rigshospitalet in Denmark. “Our results show that you should feel free to administer the oxygenation strategy best suited for the patient.”
GLP-1 analog exenatide did not show benefit during cardiac surgery
Infusion with the GLP-1 analog exenatide initiated before cardiopulmonary bypass-assisted coronary artery bypass grafting and/or surgical aortic valve replacement did not improve outcomes, according to a second independent co-primary endpoint investigated in the GLORIOUS trial.
The 2-by-2 single-center, event-driven trial randomized 1,400 patients undergoing elective or subacute coronary artery bypass grafting and/or surgical aortic valve replacement from 2016 to 2021 to a six-hour and 15-minute infusion of 17.4 micrograms of the GLP-1 analog exenatide or placebo initiated after anesthesia prior to surgery in a double-blind fashion.
“Based on a number of preclinical studies from 2010 to 2015 in stroke and myocardial infarction, which showed that treatment with exenatide could reduce final cerebral and myocardial infarction size, we had hypothesized that initiating a novel treatment of exenatide could prevent some of the organ damage that occurs during cardiopulmonary bypass-assisted heart surgery,” Wiberg said.
The composite primary endpoint assessed throughout follow-up was death, renal failure requiring renal replacement therapy, stroke, new onset heart failure or any readmission for heart failure until 323 events.
Secondary endpoints included predefined safety endpoints during the index admission, such as surgical site infection, acute kidney injury, hypoglycemia, pancreatitis, a relative reduction of ejection fraction of 50% compared to baseline, reoperation for bleeding and any cause and post-surgery myocardial infarction. Additionally, re-admission for cardiovascular causes within 12 months was monitored. Results showed that perioperative exenatide treatment did not reduce mortality or morbidity from renal failure, stroke or heart failure, compared to placebo, after a median follow-up of 5.9 years. Still, the study adds to the body of evidence for cardiac surgery approaches to consider, or not. “During cardiac surgery, we have many different strategies to choose from, many of which are based on a very low level of evidence,” Wiberg said. “It’s important to evaluate some of them in a clinical setting.”
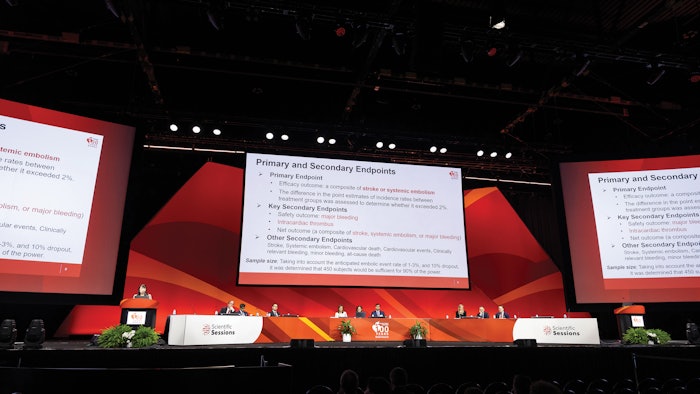
Trial shows edoxaban reduces risk of stroke or systemic embolism early after bioprosthetic valve replacement
Edoxaban, a direct oral anticoagulant (DOAC), was a safe and efficacious alternative anticoagulant therapy to warfarin early after bioprosthetic valve replacement, according to Efficacy and Safety of Edoxaban in Anticoagulant Therapy Early After Surgical Bioprosthetic Valve Replacement: the ENBALV trial. In the investigator-initiated phase 3, open label, multicenter trial, 410 patients undergoing bioprosthetic valve replacement were randomized 1:1 to edoxaban 60 mg or 30 mg daily adjusted by renal function, body weight and concomitant use of P-glycoprotein, or warfarin, with dose-adjusted monitoring prothrombin time test with an INR over a follow-up of 12 weeks after surgery; 389 patients were included in final analysis.
The primary endpoint, a composite of stroke or systemic embolism at 12 weeks after surgery, occurred in 0.5% (n=1) in the edoxaban group and 1.5% (n=3) in the warfarin group (risk difference -1.03, 95% CI, -4.34 to 1.95). Major bleeding was numerically higher in the edoxaban group (4.1% versus 1.0%, risk difference 3.07; 95% CI, -0.67 to 7.27), but no fatal bleeding or intracranial hemorrhage was observed. In the warfarin group, one fatal intracranial hemorrhage was observed.
Current guidelines recommend anticoagulant therapy with vitamin K antagonists within three to six months after bioprosthetic valve replacement to prevent thromboembolic events. Chisato Izumi, MD
Chisato Izumi, MD
“In an aging society, bioprosthetic valve replacement surgeries are increasing. Although DOACs are widely used for nonvalvular atrial fibrillation, they are not approved for early anticoagulation therapy after bioprosthetic valve replacement, including patients with sinus rhythm,” said Chisato Izumi, MD, the study’s principal investigator and a cardiologist at the National Cerebral and Cardiovascular Center in Osaka, Japan. “But our results suggest edoxaban, as an alternative anticoagulant therapy for 12 weeks after bioprosthetic valve replacement, may have clinical advantages for patients and medical staff, because patients’ conditions are largely variable during that time and edoxaban can be used with constant dose without the need for routinely monitoring anticoagulation activity. And compared to warfarin, edoxaban also has a low risk of interaction with other drugs and food, thus it is an appealing option for many patients.”
Spironolactone may reduce heart failure but did not reduce primary outcomes in patients after acute myocardial infarction
Aldosterone antagonism has been shown to reduce mortality in patients with chronic heart failure with reduced ejection fraction and in patients after myocardial infarction with overt heart failure and reduced ejection fraction. It plays a key role in reducing infarct size post-myocardial infarction and the development of heart failure. As a routine strategy, could spironolactone, an aldosterone antagonist, improve outcomes in patients with myocardial infarction but without heart failure? That was the question asked in The CLEAR SYNERGY (OASIS 9) Trial: A 2x2 Factorial Randomized Controlled Trial of Colchicine versus placebo and Spironolactone versus placebo in patients with myocardial infarction: The results of the spironolactone factorial.
The placebo-controlled factorial design trial randomized 7,062 patients with ST-elevation myocardial infarction or large non-ST-elevation myocardial infarction from 104 sites in 14 countries throughout North America, Europe, Egypt, Nepal and Australia to spironolactone 25 mg bid or placebo with enrollment between February 2018 and November 2022. Median follow-up was three years and a maximum of five years. Mean age was 60.6 years; 18% had diabetes and 9% had prior myocardial infarction. Sanjit Jolly, MD
Sanjit Jolly, MD
The co-primary outcomes for spironolactone were total composite events of cardiovascular death or new or worsening heart failure, and time-to-first occurrence of the composite of cardiovascular death, recurrent myocardial infarction, stroke or new or worsening heart failure.
Overall, spironolactone post-MI did not provide a statistically significant benefit for either primary endpoint, but a hypothesis-generating on-treatment analysis indicated a significant benefit for both primary outcomes. New or worsening heart failure declined from 2.4% to 1.6%, representing a 30% overall heart failure relative risk reduction.
“Treating patients with myocardial infarction with spironolactone was not shown to be beneficial in this trial, but our data reinforces what we already know: that spironolactone does prevent recurrent heart failure and could benefit the highest risk patients, those with myocardial infarction and heart failure,” said Sanjit Jolly, MD, the first author of the study and a scientist at the Population Health Research Institute, a joint institute of McMaster University and Hamilton Health Sciences.
Jolly noted that spironolactone has been used to treat congestive heart failure for more than 20 years. “It is underprescribed for patients with myocardial infarction and congestive heart failure because newer agents are now available, but you should still consider it for these high-risk patients,” he said. The study was simultaneously published in the New England Journal of Medicine.